Silent Voices of Immigrants and Refugees Battling with Mental Health and Addiction during COVID-19: A Follow- Up Population-Based Cohort Retrospective Study in Ontario, Canada
What is this research about?
This article investigates the disproportionate impact of the COVID-19 pandemic on immigrants and refugees in Ontario, Canada, particularly those with mental health and addiction disorders. It aims to understand how the intersection of immigration status and pre-existing mental health and addiction conditions affected COVID-19 outcomes over two years of the pandemic. This article builds on research that explored the pandemic’s impact on immigrants and refugees with mental health and addiction during the first year of COVID-19.
The article examines the compounded effects of social and clinical disadvantages, specifically focusing on the combined impact of immigration status and pre-existing mental health and addiction, on COVID-19 outcomes (vaccination rates, diagnoses, hospitalizations, ICU admissions, and mortality). It compares outcomes among immigrants with mental health and addiction to three comparison groups:
- immigrants without mental health and addiction
- non-immigrants with mental health and addiction
- non-immigrants without mental health and addiction
What do you need to know?
Immigrants and refugees often face socioeconomic disparities that increase their vulnerability to adverse health outcomes. These include low income, precarious employment, living and working in crowded spaces, immigration status, constrained social support, limited literacy of Canada’s official languages, and limited or no access to available lifesaving health care services due to systemic stigma and discrimination.
There is extensive research that highlights the impact of COVID-19 on structurally marginalized populations and individuals with preexisting mental health and addictions issues separately. However, these studies often remain unidimensional, overlooking the compounded effects of coexisting social and clinical disadvantages. This research is unique because it examines the long-term effects of the COVID-19 pandemic on immigrants living with mental health and addiction, recognizing that their financial and social resources may have been depleted over time. It also considers the shift towards digital/virtual healthcare and includes immigrants without mental health and addiction as a separate group to distinguish the differential impact of COVID-19 on those with and without social and clinical disadvantages.
What did the researchers find?
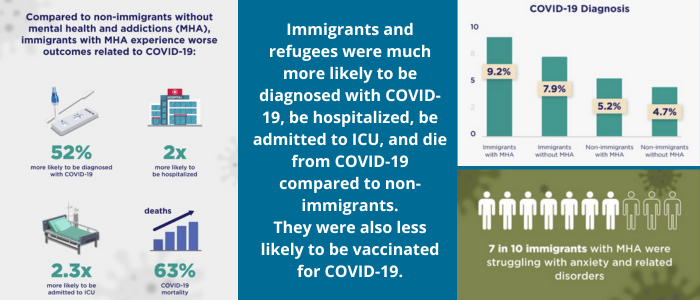
Immigrants and refugees living with mental health and addiction were 52% more likely to be diagnosed with COVID19, over twice as likely to be hospitalized and be admitted to ICU, and 65% more likely to die from COVID-19 than non-immigrants without mental health and addiction.
Additional highlights include:
- Immigrants and refugees living with mental health and addiction disorders were more socially deprived compared to non-immigrants with mental health and addiction. A significantly higher proportion of immigrants with and without mental health and addiction resided in ethnically diverse neighbourhoods.
- Immigrants with mental health and addiction were significantly more likely to be diagnosed with COVID-19, hospitalized, admitted to the intensive care unit, and die from it compared to non-immigrants without mental health and addiction.
- A clear income gradient existed across COVID-19 outcomes, with residents of the lowest-income neighbourhoods experiencing higher rates of diagnosis, hospitalization, ICU admission, and mortality.
- COVID-19 vaccination uptake dropped dramatically after the first two doses across all cohorts. There was a more pronounced decrease among immigrants.
- Immigrants from Latin America and the Caribbean were at higher risk of adverse COVID-19 outcomes.
- The Family Health Team primary care model had a protective effect.
How can you use this research?
Policymakers: Develop targeted upstream policies and community-based support systems that address the specific needs of structurally and clinically marginalized populations. This includes prioritizing these groups in future crises and implementing culturally sensitive and linguistically appropriate preventive measures.
Healthcare providers: Understand the compounded social and clinical disadvantages faced by immigrants, particularly ethno-racialized immigrants living with mental health and addiction disorders. This should inform the development of more equitable and effective healthcare interventions.
Community organizations: Work with healthcare providers to implement targeted, culturally specific outreach, education, and care strategies, such as community ambassadors/champions and pop-up clinics, to reach marginalized populations in high-need areas.
Researchers: Further explore the impact of COVID-19 on specific subgroups of immigrants, such as recent immigrants and those with different types of mental health and addiction. Future research should also address the association between vaccine uptake and other sociodemographic determinants of health, such as food security and drug use.
Future research should address the association between vaccine uptake and other sociodemographic determinants of health such a food security, length of stay or drug use, and assess the impact of COVID-19 by type of mental health and addiction (i.e. Psychotic disorders, non-psychotic disorders and substance use disorders).
What did the researchers do?
Researchers’ initial study covered the first two waves of COVID-19. A follow up retrospective cohort was conducted using linked Ontario-based administrative databases to expand the timeframe. The study period spanned from March 31, 2020, to December 31, 2021.
The study cohort included 10,356,878 Ontario residents aged 18 or older. 24% of this population were identified as immigrants and 8.9% lived with mental health and addiction. Researchers used descriptive statistics and logistic regression models to analyze the data, adjusting for various socioeconomic and health-related factors.
Stakeholders consulted included:
- Immigrants and refugees with and without mental health and addiction
- Canadian-born residents with and without mental health and addiction
- Residents from different regions of origin and residence in Ontario
- Individuals from various income quintiles and neighbourhood marginalization levels
- Patients enrolled in different primary care models
Study authors and journal/book name
Authors: Vahabi M, Matai L, Lofters A, Rayner J, Damba C, Janczur A, Kopp A, Fung K, Narushima M, Hawa R Datta G, Tharao W, Wong JP
Publication: Journal of Environmental Science and Public Health, 8 (2024): 150-167
Related Access Alliance Activities
The Disproportionate Impact of COVID-19 on Immigrants and Refugees with Chronic Illnesses
This community-based research project delved into the compounded effects of the COVID-19 pandemic on immigrants and refugees living with cancer, and mental health and addiction disorders. The study, a collaboration including Access Alliance, sought to understand the challenges faced by individuals at the intersection of social and clinical disadvantage during a public health crisis. The central question guiding the research was: What happens to those who are at the intersection of social and clinical disadvantage during a pandemic?
Impact of Social Isolation on Refugee Children and Youth
This project aims to assess the impact of social isolation on refugee youth in Toronto (Canada) as well as their coping mechanisms to overcome the adverse effects on their health and wellbeing. This will be done by conducting a rigorous systematic review of existing literature followed by peer-led facilitated discussion.
Client Perspectives on the Impacts of COVID-19
Recognizing the significant changes and challenges facing the centre and our community a year into the COVID-19 pandemic in Toronto, Access Alliance initiated a strategic planning process in the spring of 2021. To fully understand the situation, we needed to engage directly with our service-users. We conducted seven virtual focus groups between April 8 and 21, 2021 (using the Zoom platform). A total of 64 community members took part, including people of various genders, ages, education levels, sexual orientations, and cultural backgrounds.
Vaccine Engagement Impact Report
Taylor Massey-Oakridge-Victoria Village was one of the least vaccinated neighbourhoods during the summer/fall of 2021. With a coordinated effort between the partners, we raised the vaccination rate above the City’s average and significantly reduced the COVID-19 hospitalization rates during the pandemic peak.
Vaccine hesitancy among Syrian refugee parents in Canada: A multifaceted challenge in public health
This multi-country multi-institute study, housed at Access Alliance, investigates vaccine hesitancy among Syrian refugee parents in Canada. Researchers examined the factors that influence their willingness to accept COVID-19 vaccination.
